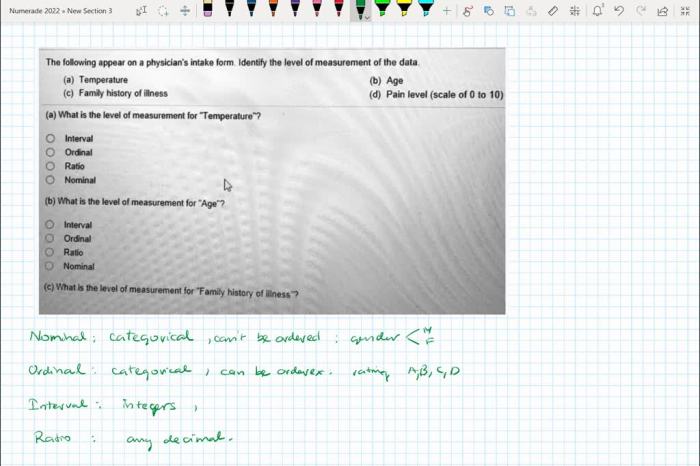
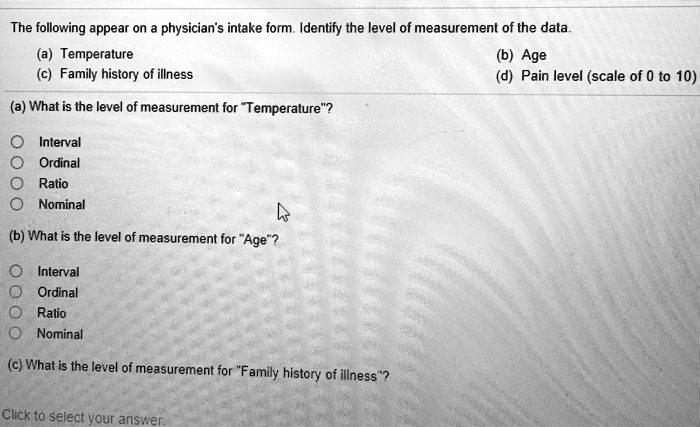
The following appear on a physician’s intake form, which serves as a vital tool in gathering comprehensive patient information to facilitate personalized care and optimize health outcomes.
This document captures crucial patient demographics, medical history, current symptoms, social history, family history, review of systems, physical examination findings, and assessment and plan, providing a holistic view of the patient’s health status.
Patient Demographics
Collecting basic information such as name, age, and contact details is essential for effective patient care. This data allows healthcare providers to:
- Identify patients accurately.
- Establish communication channels.
- Personalize treatment plans based on age-related factors.
- Track patient outcomes and monitor progress.
Maintaining patient confidentiality is crucial to protect privacy and build trust.
Medical History
Medical history includes information about past illnesses, surgeries, and medications. Gathering this data helps healthcare providers:
- Identify potential health risks.
- Rule out differential diagnoses.
- Avoid unnecessary tests or treatments.
- Establish a baseline for future comparisons.
Different types of medical history include:
- Personal medical history
- Family medical history
- Social history
Current Symptoms
Asking patients to describe their current symptoms is crucial for:
- Identifying the chief complaint.
- Determining the severity and duration of symptoms.
- Assessing potential causes and risk factors.
- Developing a differential diagnosis.
Common symptoms included on an intake form may include:
- Pain
- Nausea
- Fatigue
- Shortness of breath
- Skin changes
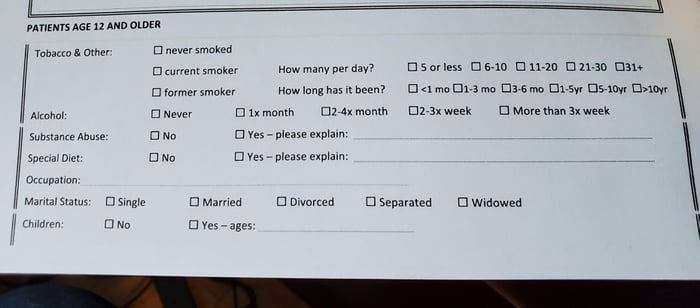
Social History
Social history includes information about occupation, lifestyle, and family relationships. This data provides insights into:
- Occupational hazards and exposures.
- Lifestyle factors that may impact health (e.g., smoking, alcohol use).
- Social support systems and potential stressors.
- Living conditions and environmental factors.
Family History: The Following Appear On A Physician’s Intake Form
Collecting information about a patient’s family history is important for:
- Identifying inherited genetic conditions.
- Assessing risk for developing certain diseases (e.g., cancer, heart disease).
- Developing preventive measures and early screening strategies.
Common genetic conditions that can be inherited include:
- Cystic fibrosis
- Sickle cell disease
- Hemophilia
Review of Systems
A review of systems is a systematic inquiry into the function of various body systems. It helps identify potential health problems by:
- Assessing symptoms related to specific body systems.
- Eliciting information about past or present medical conditions.
- Detecting subtle changes or abnormalities.
Common body systems included in a review of systems are:
- Cardiovascular system
- Respiratory system
- Gastrointestinal system
- Genitourinary system
Physical Examination
Physical examinations involve a systematic assessment of the patient’s physical health. Different types of physical examinations include:
- General examination
- Focused examination
- Comprehensive examination
Vital signs (e.g., blood pressure, temperature) are documented to assess overall health status.
Specific examination techniques are used to evaluate different body systems, such as:
- Auscultation (listening to sounds)
- Palpation (feeling)
- Percussion (tapping)
Assessment and Plan
The assessment and plan section of an intake form summarizes the findings from the patient’s history and physical examination.
- Assessment: A statement that concisely describes the patient’s current health status.
- Plan: A list of specific actions or interventions recommended to address the patient’s health concerns.
Clear and concise documentation in this section is essential for effective communication and coordination of care.
FAQ Overview
What is the purpose of a patient intake form?
A patient intake form serves as a comprehensive record of a patient’s health information, enabling healthcare providers to make informed decisions regarding diagnosis, treatment, and ongoing care.
What are the benefits of using a standardized patient intake form?
Standardized intake forms ensure consistency in data collection, facilitating efficient patient registration, accurate documentation, and enhanced communication among healthcare team members.
How can patient intake forms improve patient care?
By providing a detailed overview of a patient’s health history, intake forms empower healthcare providers to personalize treatment plans, identify potential health risks, and address specific patient needs.